 For those people who struggle with the idea of MEDICINE and STORY fitting together
For those people who struggle with the idea of MEDICINE and STORY fitting together
Modern medicine often provides only limited help in chronic health problems.
Why is this?
Let’s work on an actual example of meaning-full disease, which clearly shows the way medicine and story go hand-in-hand. (If you want to press on with the MAIN ROUTE we tell the same story there too.) BACK TO MAIN ROUTE>>

Patient T, aged 55, requests help because she wants to ‘live life more fully’. In her 30’s she developed leukoplakia, a precancerous condition of the mouth. By the time she came to me she had had 7 surgical interventions, including removal of cancer of the mouth, and plastic reconstructions of the tongue and the floor of the mouth–the last requiring 18 months rehabilitation as she learned to speak again. Early in the interview she proffered the interesting comment that “if only I could get rid of it I would be able to live more fully from day to day”. Though she was obviously (!) referring to the leukoplakia and cancerous tendency I suspected the it was not the cancer which had been removed 2 years before, with no evidence of recurrence. I noted the words but made no comment.
A review of her life-story was illuminating. Apparently, after she was born, she and her mother were collected by father from the hospital. He dropped them off at home and went off to see his mistress. When T. was 7 years old her father suicided, though she was not aware of the nature of his death. At age 12 she was crying in her bedroom. Mother found her, asked what was wrong, and T. replied she was crying about “Daddy”. Mother, who was now alcoholic, responded: “It’s your fault your father is dead–you would never sit on his knee.” The background to this cruel comment is not entirely clear. T. did remember that as a child she often felt much more identified with her absent father than with her mother. At age 16 she learned from relatives that her father had suicided. At 19 she entered a marriage that, over 6 years, repeated in some ways the traumas of childhood. At age 33 she developed the leukoplakia of the mouth. It turns out that this was the age that her father suicided. Her father was an oral surgeon. I pointed this out to T. who had herself wondered, over the years, whether this was significant, though it had never been discussed with doctors. Returning in my mind to the it referred to above, I asked her what, apart from this cancerous tendency, she would most like to get rid of in her life.
She seemed to understand what I was asking, but struggled initially, becoming very tearful, unable to find the right word. Eventually she said she most wanted to get rid of the shame. To me it seemed likely that the shame and the precancerous leukoplakia were intimately connected.
Lots of questions ran through my mind. If this woman’s story had been known, and taken seriously, when she was 33, and if the shame had been resolved, would she have run the same clinical course? Would this cancerous tendency remit if she did some appropriate therapy? In fact she did do some brief psychotherapy, lasting only nine sessions. A year later she reported no further problems and her surgeon expressed some astonishment with the good state of her mouth. Perhaps more compelling is that the turning point in the psychotherapy occurred when she actually started to remember sitting on her father’s knee. She reported a persistent “joy” starting immediately after the session in which that memory surfaced. The joy persisted, and seems to have expressed itself in a variety of interpersonal and social freedoms. She also reports now that for the first time in her life she finds herself considering living into her eighties.
CAN YOU SEE THE PROBLEM THAT MODERN MEDICINE WOULD HAVE WITH THIS STORY? A FEELING LIKE SHAME CAUSING PRECANCER AND THEN CANCER OF THE MOUTH IS JUST NOT CONCEIVABLE IN MODERN MEDICINE.
WHY IS THIS?
BECAUSE WESTERN MODELS OF DISEASE DO NOT ALLOW IT.
This is complicated territory for those who are interested in theory. If this is you then print this off-it will be easier to read!
In Western medicine there are two favored ways of looking at disease.
 The first is the BIOMEDICAL model.
The first is the BIOMEDICAL model.
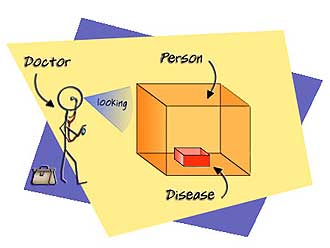
Using the biomedical model we tend to describe a disease as an ‘object’, or as a ‘mechanical’ dysfunction in an object (in a body).
In biomedical terms this boils down to preoccupation with physical structure and function–genetics, biochemistry, anatomy, histopathology, pathophysiology, physical signs, and symptoms.
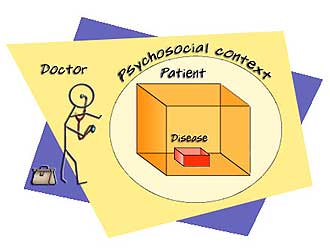
The second uses the BIOPSYCHOSOCIAL model.
The biopsychosocial model (Engel, 1977) is a more recent improvement and enlargement of the biomedical model. It adds wider contextual influences to the limited biomedical view of disease.
The biomedical model sees the patient as a biological machine, while the biopsychosocial model sees the patient as a machine in a wider psychosocial context. The latter takes more of our lives into account than does the biomedical model.
The problem is that we see many examples of diseases clearly associated with highly specific meanings and stories, and neither of these models (in the ways they are typically applied) accommodate these very specific connections.
Why not?
The biomedical model has no room for meaning in disease
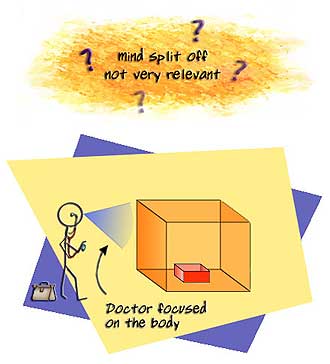
The biomedical model simply does not allow for personal meaning or story as being part of the causation of disease. Mind and body are dealt with as entirely separate. This means, of course, that mind and brain are separate entities as well.
In this model with its assumption of separateness, matter and meaning cannot occupy the same stage, or, if they do, it is only because matter is fundamental and mind and meaning are derivative; they are epi-phenomena which ultimately reduce to matter. As such mind and meaning are peripheral to our interests as biomedical clinicians. This is why many physicians show little interest in the other things going on in your life when your illness begins.
By far the majority of doctors (even if they are sympathetic to a wider view) work from this biomedical model.
Some people believe we are rescued by the biopsychosocial model. But the biopsychosocial model fails to accommodate highly specific meaning.
The biopsychosocial model appears to provide a place for ‘story’ and in many ways it does. But actually it cannot explain the very specific ‘story’ of shame associated with mouth cancer given in Scenic route 1. Why can’t it? In its most popular version it connects life story and disease by calling on (hold your seat!) the mechanisms of psycho/neuro/endocrino/immunology. It invokes linkages and networking between various systems (hence the term psycho/neuro/endocrino/immunology) which, while appearing quite broad, have severe limitations.
In a nutshell, the biopsychosocial model cannot explain the stories given in this program.
Its capacity to accommodate highly specific meaning in the form of disease (for instance the shame and cancer case) along psychoneuroendocrinoimmunological lines collapses at two crucial and major hurdles.
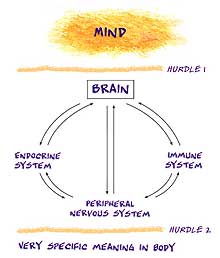
Firstly, it must solve the mind-to-brain problem if it is to explain the conversion of complex personal meanings generated (according to the biomedical model) in the split-off mind).
Secondly, once a meaning has been converted into a brain activity it must solve how the nervous, immune, and endocrine systems can possibly project such complex meanings out to the periphery of the body so as to produce obvious somatic metaphors.
Even if we could solve the mind/body(brain) problem (the first hurdle) we cannot see where in our knowledge of the endocrine, immune, or peripheral nervous systems there is a capacity for projecting extremely complex meaning into an exquisitely appropriate and unique physical disease form (the second hurdle). The biopsychosocial model cannot do this because it relies on the capacities of the immune, endocrine, and peripheral nervous system for bodily effects. These bodily systems can of course mediate nonspecific organ effects but not the translation (into bodily form) of the exquisitely specific complex meaning we see in the many examples on this website.